Cause & Spread
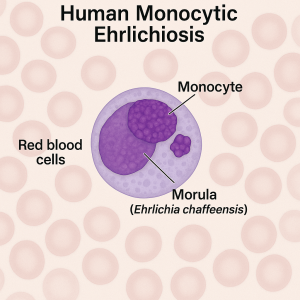
Ehrlichiosis is kind of a tongue-twister and not as well-known as Lyme, but it’s an important tick disease in the U.S. It is actually a name for a group of diseases caused by bacteria in the genus Ehrlichia. The primary one in the U.S. is Ehrlichia chaffeensis, which causes Human Monocytic Ehrlichiosis (HME). There’s also E. ewingii (which can cause illness in people, especially those with compromised immunity) and E. muris eauclairensis (found in the upper Midwest). Ehrlichia bacteria live inside blood cells (specifically white blood cells). How do you get infected? Through the bite of an infected tick, of course. The Lone Star tick (Amblyomma americanum) is the main vector for ehrlichiosis in the U.S. This tick is very common in the southeastern and south-central states (think states like Missouri, Arkansas, Oklahoma, the Carolinas, Georgia, Tennessee, Virginia, Texas – basically from the East Coast extending westward to Texas. Lone Star ticks are aggressive biters (they don’t shy away from human blood!). When an infected Lone Star tick bites you, it can transmit Ehrlichia bacteria. There’s also a rarer form of ehrlichiosis in the upper Midwest (Wisconsin/Minnesota) caused by E. muris eauclairensis, which is actually carried by the blacklegged tick. But the large majority of cases come from the Lone Star tick in southern/central regions. Ehrlichiosis can (very rarely) be transmitted via blood transfusion or organ transplant, because the bacteria live in blood cells. But this is uncommon. You can’t catch it from another person casually; it really comes down to tick bites.
Symptoms
Ehrlichiosis typically hits you 1-2 weeks after the tick bite. The symptoms are usually flu-like at first and pretty non-specific: fever, chills, severe headache, muscle aches, and often nausea or other tummy troubles (vomiting, diarrhea, loss of appetite). Some people might have confusion. One hallmark that sometimes occurs is a rash, but here’s the tricky part: rash in ehrlichiosis is not super common in adults – it’s more often seen in children (and in infections caused by E. chaffeensis). When rash does occur, it usually appears a few days into the illness (around day 5) and can look like red splotches or tiny pinpoint dots. In fact, less than half of adult patients get a rash, so don’t rule out ehrlichiosis just because there’s no rash. Think of ehrlichiosis as a nasty summer flu with possible rash. If not treated promptly, ehrlichiosis can become severe. Delayed treatment can lead to serious complications like damage to the brain or nervous system (encephalitis), respiratory failure, uncontrolled bleeding, organ failure, and unfortunately it can be fatal in some cases. People over 50 or with weakened immune systems are at higher risk for severe outcomes. So we really want to catch this one early.
Diagnosis
Because early symptoms are generic (fever, headache, etc.), ehrlichiosis can be tricky to diagnose. Doctors who are aware of tick diseases will consider ehrlichiosis if you have a compatible illness in spring/summer and were in areas with ticks. Blood tests can help: there’s a PCR test that can detect Ehrlichia DNA in the blood, and there are antibody tests (IFA) that look for your immune response. Early on, the PCR is useful if positive (later on, antibody tests can confirm). Often, if ehrlichiosis is suspected, a doctor will start treatment before lab results come back. This is common practice, because waiting for confirmation could be dangerous. Sometimes clues in routine bloodwork hint at ehrlichiosis: low white blood cell count, low platelets, and elevated liver enzymes (those are common in this infection).
Treatment
The great news is that ehrlichiosis is very treatable with antibiotics. The go-to treatment (and really the only one you should use) is doxycycline, the same antibiotic used for Lyme, but here it’s truly the lifesaver. Doxycycline is recommended for adults and children of all ages with suspected ehrlichiosis. Yes, it’s even given to young kids in this case (while doxycycline can cause tooth staining in children with longer courses, the risk from a short course is low and ehrlichiosis is dangerous enough that we don’t hesitate to use it). Typically, a course of about 7-10 days of doxycycline will cure ehrlichiosis. Often doctors will continue treatment for at least 3 days after the fever goes away. Most people recover quickly if they start doxycycline early. Sometimes within 24-48 hours they feel much better, which is a big hint that it was ehrlichiosis. It’s important to start treatment as soon as ehrlichiosis is suspected, even without waiting for lab results, because early treatment can prevent severe illness or death. There’s no effective alternative antibiotic – Ehrlichia are intracellular bacteria (meaning they live inside your cells) and doxycycline is excellent at clearing them. So if a doctor thinks you have ehrlichiosis, you’ll get doxycycline. If you respond fast, that often clinches the diagnosis. After recovery, you don’t usually have long-term problems. Unlike Lyme, there’s no chronic form of ehrlichiosis. And currently, there’s no vaccine, so prevention (tick bite avoidance) is key.
Bottom line: The earlier you tret it the better. And once the bacteria are gone, they’re gone.